Key Takeaways
- Stress and glucose spikes go hand in hand, as cortisol levels increase as part of the fight-or-flight response.
- There are a variety of cortisol control strategies available, including sleep anchoring, breathwork, and meal sequencing.
that {{mid-cta}}
Fall and early winter are peak stress seasons. With end-of-year deadlines, holiday prep, and immune challenges, cortisol increases, which also raises blood sugar levels.
Understanding stress and glucose spikes can help prevent both blood sugar swings and burnout. Continue reading to learn more about cortisol control strategies for optimal glycemic control.
Cortisol and Metabolism: The Science Behind Stress Spikes

Cortisol is a steroid hormone. It helps manage metabolism, inflammation, and glucose levels.
Cortisol and metabolism are related, as cortisol controls how the body uses fat, protein, and carbohydrates. It affects blood sugar by stimulating the liver to produce glucose. In turn, stress-induced blood glucose spikes can occur.
Insulin is also affected by cortisol, as chronic high levels of cortisol make it harder for the body to use insulin properly. This is known as insulin resistance.1 Short-term and chronic stress affect the body differently. Acute stress usually comes from temporary stressors or difficult situations. The fight-or-flight response triggers short-term changes in the body, such as an elevated heart rate and the release of stress hormones, including adrenaline.
Chronic stress occurs when a stressor persists over a long period of time. It is the most common cause of elevated cortisol levels.2 The effects of stress are many; it impacts physiological and psychological health, which increases the risk of developing cardiovascular disease, anxiety, depression, and other health conditions.3
Cortisol also plays a role in food intake and cravings. It stimulates appetite and promotes intake of high-energy, desirable foods. This is because the body needs enough energy for the fight-or-flight response.4
Another effect of cortisol is weight gain due to insulin resistance and muscle breakdown. Decreased muscle mass can slow down metabolism, making it easier to gain weight. Increased fat storage, especially in the abdominal area, is another side effect of high cortisol levels.2
Work Deadlines and Seasonal Stressors

Fall and winter can be especially stressful with an increased workload and time pressure associated with end-of-year deadlines. These stressors can increase cortisol levels.
This time of year is also when people tend to experience immune season fatigue. Stress can negatively impact the immune system by suppressing certain immune cells and altering cytokine production. As a result, the body can’t fight infections as well as it normally can.5
Between holiday events and work deadlines, it’s easy to overcommit and spread yourself thin. This can increase work stress, raise glucose levels, and wreak havoc on metabolic health.
The Metabolic Playbook: Strategies to Mitigate Stress Spikes

Stress management for metabolism is crucial. Fortunately, there are many ways to reduce stress.
- Add physical activity to your routine, even in small amounts. Cardio and stretching can reduce cortisol levels.
- Focus on meal sequencing and timing. Eat protein and fiber-containing foods first to prevent post-meal cravings.
- Sleep anchoring and maintaining consistent sleep and wake times help stabilize cortisol levels.
- Breathwork and mindfulness are helpful, especially in stressful situations. Practice deep breathing exercises for 2-5 minutes during high-stress moments.
- Make changes to your environment by adjusting your exposure to natural light and using ergonomic products.
- Connect with others to stay social and be surrounded by supportive people during stressful situations.
- Set boundaries and learn to delegate tasks to avoid becoming overwhelmed by overcommitting.
- Write down your thoughts and feelings to get them out of your head and release pent-up emotions.
- Lean into hobbies, such as playing an instrument, reading, or baking, to relieve stress.
- Find a therapist who can help you manage your stress with effective coping strategies.6
- Reduce alcohol and caffeine intake, as both can raise cortisol levels.
- Talk to your healthcare provider to see if taking supplements is right for you. Magnesium and ashwagandha, for example, have been shown to support the body’s stress response.2
Using Signos to Track Stress-Related Glucose Effects
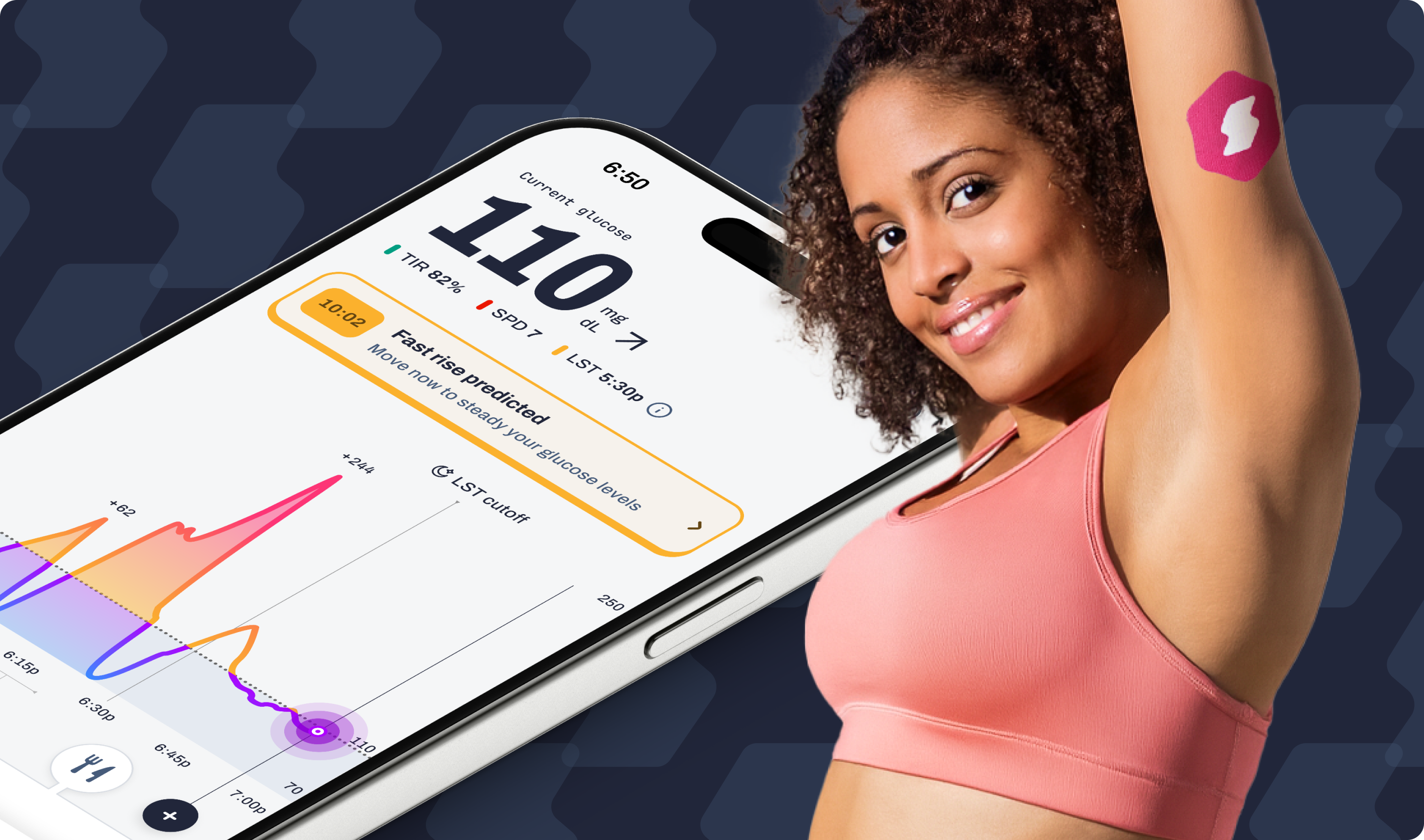
Insight from Signos can help you visualize the connections between your stress levels and internal responses in real time. With continuous glucose data, you can see how your body responds during high-pressure moments, emotional triggers, or recovery periods. You can also experiment with different stress-management techniques to find what works best for you.
Try These CGM Experiments:
1. Morning Mindfulness vs. Rushed Start
- What to do: Compare two mornings: one where you start the day calmly (with meditation or deep breathing) and one where you rush straight into emails or work.
- What to watch: Does your glucose stay more stable on mindful mornings? Many members find that even 5–10 minutes of breathwork before breakfast leads to flatter curves.
2. Workout Timing and Stress Relief
- What to do: Track glucose on a stressful day when you take a brisk walk or do a short workout during lunch versus a day when you skip it.
- What to watch: Does movement help bring glucose back to baseline faster? Exercise often blunts cortisol and helps clear stress-induced glucose from the bloodstream.
3. Post-Stress Meal Response
- What to do: Eat the same meal after a calm afternoon one day and after a stressful meeting another day.
- What to watch: Do you see a higher or longer glucose spike after stress? This can show how stress hormones alter digestion and glucose tolerance.
4. Evening Wind-Down Routine
- What to do: Try a relaxing bedtime ritual (stretching, journaling, or breathing) versus scrolling or working late.
- What to watch: Look at your overnight glucose curve. Users often find fewer late-night spikes and better morning stability after relaxation habits.
5. Caffeine and Stress Interaction
- What to do: On a low-stress day, have your normal coffee and track your glucose. Then try the same on a high-stress day.
- What to watch: Stress and caffeine can amplify each other’s effects. Some members see sharper glucose peaks when both are present.
Real-life support from Signos’ registered dietitians can help you interpret your patterns and identify personalized interventions, whether that’s adjusting meal timing, refining recovery habits, or integrating stress-mitigation strategies. The goal: to flatten glucose curves, build resilience, and improve metabolic health from the inside out.
The Bottom Line
While fluctuations in stress levels are unavoidable, the metabolic impact is manageable. By practicing small, effective strategies, you can stabilize blood glucose, reduce the risk of burnout, and support your immune system.
Signos empowers readers to understand how stress impacts metabolic health while making it easier to adapt daily routines for resilience and improved well-being.
Learn More With Signos’ Expert Advice
Signos offers 24/7 glucose monitoring, support from registered dietitians, food logging, and personalized AI insights to help you achieve better health. To learn more about the role of glucose in overall wellness, visit Signos’ blog.
Topics discussed in this article:
References
- Iiu, T. (2024). The stress hormone: How cortisol affects diabetes outcomes and its managing and monitoring. Diabetes manag, 14(5), 663-664. https://www.openaccessjournals.com/articles/the-stress-hormone-how-cortisol-affects--diabetes-outcomes-and-its-managing-and--monitoring.pdf
- Singh B, & Maurya NK. (2024, March 28). The cortisol connection: Weight gain and stress hormones. Arch Pharm Pharma Sci, 8, 009-013. doi:10.29328/journal.apps.1001050
- Chu B, Marwaha K, Sanvictores T, Awosika, A.O., & Ayers, D. (Updated 2024, May 7). Physiology, Stress Reaction. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541120/
- Chao, A. M., Jastreboff, A. M., White, M. A., Grilo, C. M., & Sinha, R. (2017). Stress, cortisol, and other appetite-related hormones: Prospective prediction of 6-month changes in food cravings and weight. Obesity (Silver Spring, Md.), 25(4), 713–720. https://doi.org/10.1002/oby.21790
- Alotiby, A. (2024). Immunology of Stress: A Review Article. Journal of Clinical Medicine, 13(21), 6394. https://doi.org/10.3390/jcm13216394
- Mayo Clinic Staff. (n.d.). Stress management.Mayoclinic.org. https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/stress-relievers/art-20047257




.svg)










.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
