Key Takeaways
- Reactive hypoglycemia is a sudden drop in blood glucose levels a few hours after eating, often causing shakiness, lightheadedness, and fatigue.
- Causes range from too much insulin after carb-heavy meals to underlying conditions like type 2 diabetes or gastric bypass surgery.
- Eating balanced meals with whole grains, protein, and fiber can help prevent glucose crashes and support steady energy.
{{mid-cta}}
Ever felt shaky, anxious, or ravenously hungry just a couple of hours after eating? That post-meal crash can feel like betrayal; you just fueled up, so why does your body act like it’s running on empty?
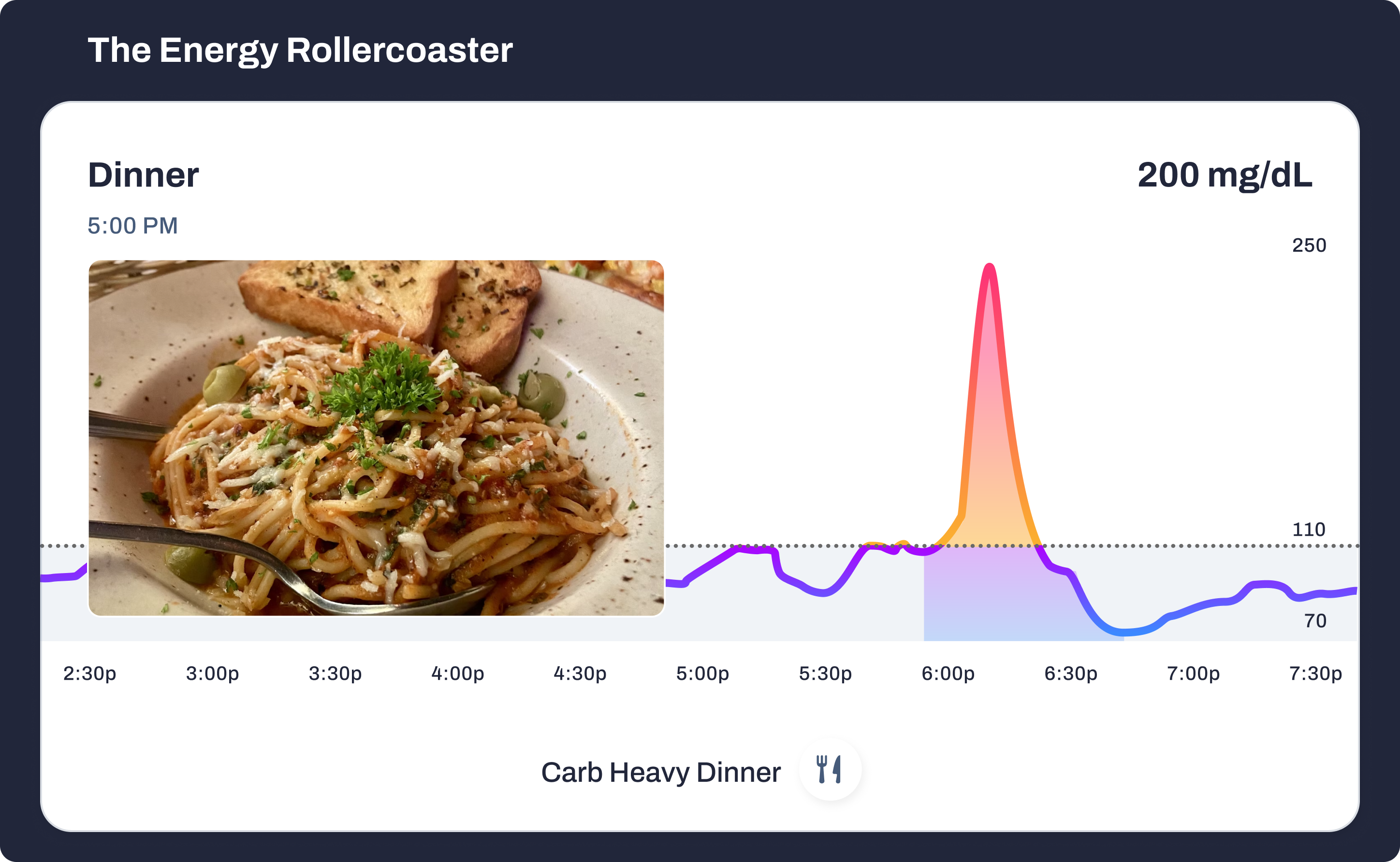
Here’s the thing: not every dip in blood glucose is dangerous. After a carb-heavy meal, it’s normal for glucose levels to rise, then fall as insulin does its job. But there’s a difference between a gentle slope and a freefall.
- Normal dip: Glucose rises, insulin helps clear it, and levels return smoothly toward baseline.
- Reactive hypoglycemia (postprandial hypoglycemia): Glucose levels drop too far, too fast, often below 70 mg/dL (3.9 mmol/L). That’s when symptoms like shakiness, lightheadedness, or irritability strike.
Let’s break down what causes these crashes, how to recognize the red flags, and what you can do to stabilize blood sugar levels with smart, metabolic strategies.
Reactive Hypoglycemia, Explained
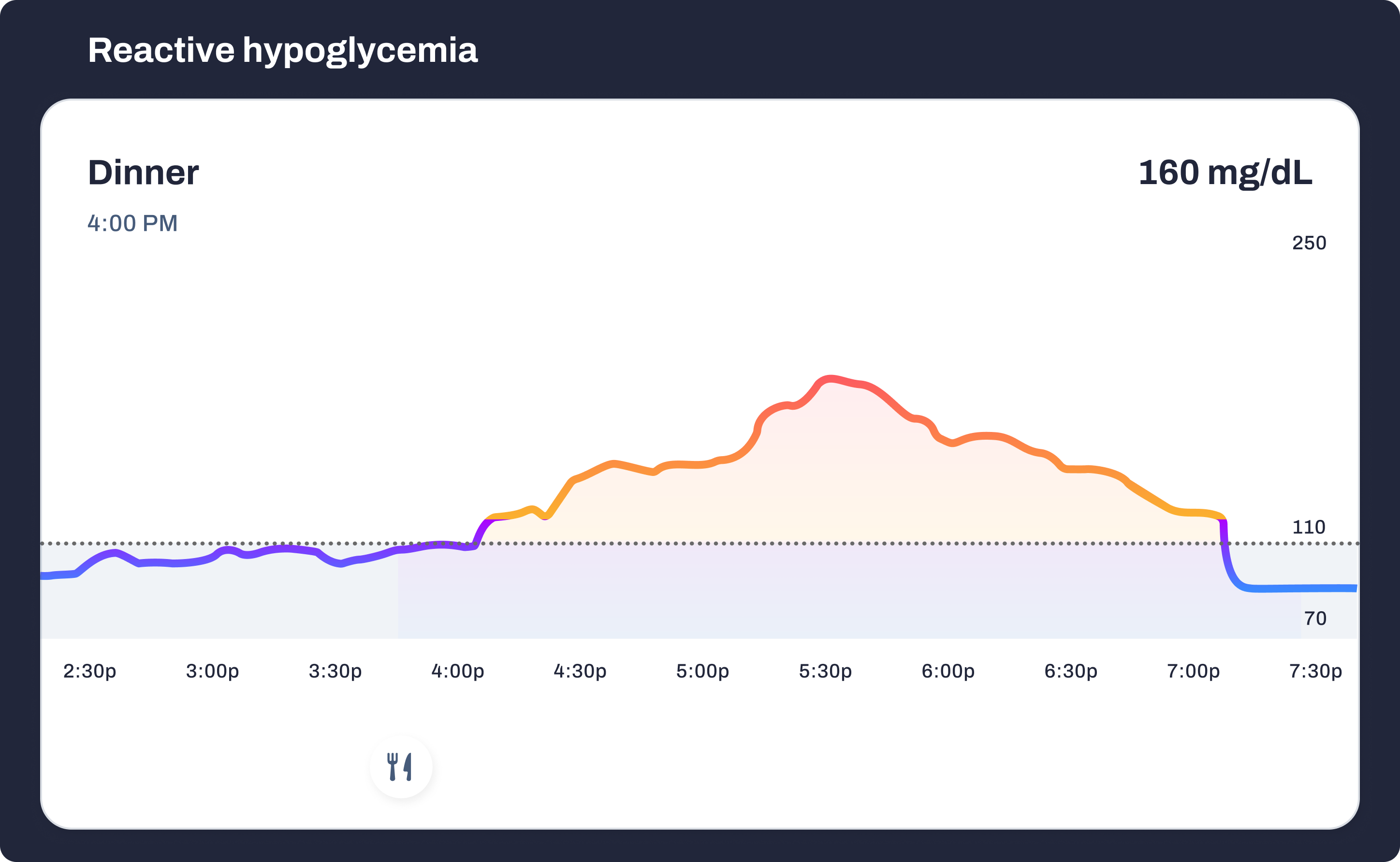
Reactive hypoglycemia (also called postprandial hypoglycemia) happens when blood glucose levels drop too far within 2 to 4 hours of eating.1 It’s not the same as fasting hypoglycemia, which occurs after going long periods without food. Instead, it’s tied directly to how your body responds to a meal.1
Here’s what’s going on: you eat, your pancreas releases insulin to help shuttle glucose into your cells, but in some cases, the system overshoots. Too much insulin hangs around, and instead of returning to baseline, your blood sugar levels sink below where they should be. That dip (sometimes dipping under 70 mg/dl (3.9 mmol/l)) can trigger symptoms that make you feel shaky, weak, or foggy.1
Why does it happen? Common culprits include:
- Excessive insulin release: Some people’s systems are hypersensitive to carbs. A bowl of pasta or soda floods the bloodstream with glucose, and the pancreas responds by pumping out excessive insulin.2 The result? Levels crash lower than your body can comfortably handle.
- Insulin resistance/prediabetes: In the early stages of type 2 diabetes, insulin isn’t as effective. Your body may release more of it to compensate, but because the response is poorly timed, glucose still drops in an unsteady way.2
- Gastric bypass or weight-loss surgery: When food moves rapidly into the small intestine, it can spark a surge of insulin secretion. This “dumping syndrome” is a well-documented cause of reactive hypoglycemia in people who’ve had gastric bypass.3
- Refined carbs and sugary foods: Meals built around white bread, pastries, or soda break down fast, spiking glucose before it plummets. Without protein, fiber, or healthy fats to slow absorption, your body is set up for the spike-crash cycle.
- Other endocrine conditions: Though less common, deficiencies in hormones like cortisol or glucagon (both critical in stabilizing blood glucose levels) can set the stage for reactive dips.4 This is why endocrinology specialists often evaluate unexplained crashes.
Reactive hypoglycemia isn’t always a chronic condition. Sometimes it’s situational, linked to what you ate, how much you slept, or even stress hormones. But repeated dips may signal an underlying metabolic imbalance worth exploring with your healthcare provider.
Symptoms of Reactive Hypoglycemia
Reactive hypoglycemia doesn’t whisper; it announces itself. These “hypos” come on quickly, sometimes within a couple of hours of eating, and they can disrupt your day in minutes.
Classic symptoms include:
- Shakiness or trembling: A hallmark sign that glucose is running low and your body is flooding with stress hormones like adrenaline.
- Lightheadedness or dizziness: A signal that the brain isn’t getting steady fuel.
- Sweating, racing heartbeat: The body’s “fight or flight” response kicks in to restore balance.
- Irritability, anxiety, or sudden mood changes: Rapid glucose shifts affect neurotransmitters, leaving you edgy or on edge.
- Intense hunger or carb cravings: Your body’s emergency response: eat fast, simple fuel.
- Difficulty concentrating or brain fog: Low glucose means the brain has to ration energy, so tasks feel harder.
- Loss of consciousness (rare): In more extreme or untreated cases, low blood glucose can progress to fainting or even seizures, though this is far more common in type 1 diabetes than in reactive hypoglycemia.
What makes these symptoms tricky is that they’re easy to brush off as “stress,” “a bad lunch choice,” or “just being tired.” But if they reliably appear after meals, your body may be showing you the symptoms of reactive hypoglycemia in real time.
How It Impacts Metabolism and Energy
A reactive dip isn’t just a passing annoyance; it has ripple effects across your energy, mood, and metabolic health.
- The Energy Rollercoaster: After a carb-heavy meal, glucose spikes, then plunges. This seesaw leaves you fatigued and unfocused. Over time, the cycle can erode productivity and make daily energy unpredictable.
- Mood and Cravings: Glucose crashes can feel like an emotional ambush. Irritability, anxiety, and sudden carb cravings are common because the brain interprets low glucose as a threat and demands quick fixes like sugar or caffeine. This often fuels the cycle of sugary foods, spike, crash, cravings, then repeat.
- Endocrine Stress: Frequent hypos may not mean you have diabetes mellitus, but they do tax the system. Insulin sensitivity can change, and the constant oscillation may indicate early dysfunction in how the endocrine system (including insulin, cortisol, and glucagon) works together.2 Left unchecked, these swings may increase the risk of developing type 2 diabetes later on.
Think of it as a signal flare. Your metabolism is telling you it doesn’t like being whipped around. Understanding the root cause and adjusting your food, lifestyle, or medical treatment accordingly helps you move from reactive crashes to steady, sustainable energy.
How Doctors Confirm It
Reactive hypoglycemia isn’t diagnosed by vibes or by guessing based on how shaky you feel after lunch. It requires clinical testing and interpretation by a healthcare professional. Because symptoms can overlap with anxiety, stress, or other conditions, testing helps separate a true glucose issue from look-alikes.
Common tools include:
- Oral Glucose Tolerance Test (OGTT): After drinking a glucose-heavy solution, your plasma glucose is measured at intervals. If blood sugar spikes and then drops below 70 mg/dl (3.9 mmol/l), it may point to reactive hypoglycemia.2 That said, OGTTs aren’t perfect; they can trigger false positives in people who wouldn’t normally experience reactive dips in daily life.
- Mixed-Meal Tolerance Test: Instead of syrupy glucose drinks, this test uses balanced meals or shakes that mimic how you’d normally eat. It often gives a more realistic picture of how your pancreas and insulin secretion respond to food.2
- Continuous Glucose Monitoring (CGM): Worn on the skin, a CGM tracks blood glucose levels every few minutes. It can reveal patterns invisible to one-off lab tests, like a drop three hours after breakfast or repeat crashes after carb-heavy dinners. For many patients, this real-world data is the “aha moment” that confirms what symptoms have been hinting at.
When symptoms are frequent or severe, an endocrinologist is often brought in to rule out other causes of low blood glucose, like adrenal (cortisol) issues, insulinoma (rare tumors that produce insulin), or medication side effects. Confirming reactive hypoglycemia is less about one single test and more about pattern recognition across labs, symptoms, and history.
The Metabolic Playbook: How to Stay Steady
.png)
If reactive hypoglycemia feels like your metabolism is playing offense against you, the good news is you can flip the playbook. Stabilizing blood sugar levels doesn’t always require medication; often, it starts with smart nutrition and habit shifts.
Fuel Smarter
- Pair your carbs wisely. Don’t eat carbohydrates alone. Team them with protein, healthy fats, and fiber to blunt the glucose surge. Example: whole-grain toast with avocado and eggs instead of toast with jelly.
- Upgrade your carbs. Swap refined starches like white bread for whole grains, beans, vegetables, and low-GI fruits. These release glucose more slowly, keeping energy steady.
- Watch portion size. A plate piled high with pasta will hit harder than a smaller serving balanced with lean protein and greens.
Eat Strategically
- Small meals > big swings. Large meals can overwhelm your system. Eating smaller meals or snacks every 3–4 hours provides a steady fuel stream without overloading insulin.
- Emergency fixes done right. If blood glucose drops below 70 mg/dl, fast-acting carbs like fruit juice or glucose tablets are essential. But once you’re above 70 mg/dl again, follow up with a balanced snack (protein, fiber, and fat) to prevent another crash.
- Stay hydrated. Dehydration can worsen fatigue and dizziness. Aim for water or unsweetened beverages; skip soda or sweetened coffee drinks that cause unnecessary glucose spikes.
Spot and Adapt
- Track your own data. A CGM is one of the best ways to uncover personal triggers. You may find your glucose only dips after certain foods (say, sushi with white rice) or at certain times (like late afternoon).
- Avoid quick fixes. Candy, soda, or energy drinks can rescue you temporarily, but they almost guarantee another crash. Think of them as short-term bandages, not solutions.
- Watch lifestyle factors. Poor sleep, stress, and alcohol can all worsen reactive dips. Stress hormones, such as cortisol, directly influence glucose levels.
When Medical Treatment Matters
Sometimes lifestyle tweaks aren’t enough. If your crashes are frequent, severe, or include serious symptoms like confusion or loss of consciousness, it’s time to escalate:
- A provider may adjust medications that affect insulin sensitivity or insulin levels.
- Endocrine testing may be performed to rule out rare conditions, such as tumors or hormone deficiencies.
- Guidance from an endocrinologist can ensure you’re addressing both symptoms and root causes.
Bottom Line
Reactive hypoglycemia isn’t just about feeling shaky after a meal; it’s your body signaling that glucose regulation needs attention. While the dips can be unsettling, they’re not random. With the right testing, smarter food pairings, and consistent glucose tracking, most people can move from unpredictable crashes to a more stable, steady energy curve.
Think of it this way: instead of guessing whether that mid-afternoon crash came from your sandwich or your stress levels, continuous glucose monitoring takes the mystery out of the equation. A CGM shows the exact moment your glucose peaks and where it starts to plunge, giving you the power to adjust in real time, whether that means rethinking your breakfast, spacing your meals, or taking a short walk after lunch.
For most, lifestyle shifts such as balanced meals, strategic snacking, and tracking patterns can make a huge difference. But if your dips are frequent, severe, or don’t respond to habit changes, it’s important to bring your data to a doctor or endocrinologist. They can rule out underlying causes and personalize a treatment plan.
At Signos, we believe you don’t have to ride the rollercoaster; you can draw the line. With real-time feedback, science-backed strategies, and the tools to connect symptoms to data, you can turn reactive hypoglycemia from an unpredictable setback into a condition you manage with confidence.
Learn More With Signos’ Expert Advice
Take the guesswork out of metabolic health. Continuous glucose monitors (CGMs) track glucose, showing you how sleep, stress, meal timing, and food pairings influence your glucose patterns and daily energy.
The Signos blog is filled with opportunities to learn more about how CGMs can help you become the healthiest version of yourself.
Topics discussed in this article:
References
- Engeroff T, Groneberg DA, Wilke J. After Dinner Rest a While, After Supper Walk a Mile? A Systematic Review with Meta-analysis on the Acute Postprandial Glycemic Response to Exercise Before and After Meal Ingestion in Healthy Subjects and Patients with Impaired Glucose Tolerance. Sports Med. 2023;53(4):849-869. doi:10.1007/s40279-022-01808-7
- Kang J, Fardman BM, Ratamess NA, Faigenbaum AD, Bush JA. Efficacy of Postprandial Exercise in Mitigating Glycemic Responses in Overweight Individuals and Individuals with Obesity and Type 2 Diabetes—A Systematic Review and Meta-Analysis. Nutrients. 2023;15(20):4489. doi:10.3390/nu15204489
- Hashimoto K, Dora K, Murakami Y, et al. Positive impact of a 10-min walk immediately after glucose intake on postprandial glucose levels. Scientific Reports. 2025;15(1). doi:10.1038/s41598-025-07312-y
- Aqeel M, Forster A, Richards E, et al. The Effect of timing of exercise and eating on postprandial Response in Adults: a systematic review. Nutrients. 2020;12(1):221. doi:10.3390/nu12010221
- Hosseini-Asl MK, Taherifard E, Mousavi MR. The effect of a short-term physical activity after meals on gastrointestinal symptoms in individuals with functional abdominal bloating: a randomized clinical trial. Gastroenterol Hepatol Bed Bench. 2021;14(1):59-66.
- Vahratian A, Blumberg SJ, Terlizzi EP, Schiller JS. Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID-19 pandemic — United States, August 2020–February 2021. MMWR Morbidity and Mortality Weekly Report. 2021;70(13):490-494. doi:10.15585/mmwr.mm7013e2
- Xu Z, Zheng X, Ding H, et al. The Effect of Walking on Depressive and Anxiety Symptoms: Systematic Review and Meta-Analysis. JMIR Public Health and Surveillance. 2024;10:e48355. doi:10.2196/48355
- Hatchell K MD. Does regular walking improve lipid levels in adults? | MDedge.
- Franczyk B, Gluba-Brzózka A, Ciałkowska-Rysz A, Ławiński J, Rysz J. The Impact of Aerobic exercise on HDL Quantity and Quality: A Narrative review. International Journal of Molecular Sciences. 2023;24(5):4653. doi:10.3390/ijms24054653
- McMullan S, Nguyen C, Smith DK. Can walking lower blood pressure in patients with hypertension? AAFP. 2022.
- Miller CR, Wactawski-Wende J, Manson JE, et al. Walking volume and speed are inversely associated with incidence of treated hypertension in postmenopausal women. Hypertension. 2020;76(5):1435-1443. doi:10.1161/hypertensionaha.120.15839




.svg)









.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
