Key Takeaways
- Non-diabetic users can benefit from CGMs by spotting hidden glucose spikes, optimizing nutrition, improving performance, and building metabolic awareness.
- CGMs have limitations: cost, accessibility, data interpretation, and potential emotional stress from constant tracking.
- Beyond diabetes, CGMs support better lifestyle decisions by showing how food, exercise, stress, and sleep impact your glucose patterns.
- Technology is evolving quickly with advances in smaller sensors, wearable integrations, AI-driven predictions, and broader accessibility.
{{mid-cta}}
Once upon a time, continuous glucose monitors (CGMs) were reserved for people with type 1 diabetes or type 2 diabetes, prescribed by an endocrinologist and calibrated against a fingerstick glucose meter. Fast-forward to now: you’ll see CGM sensors on athletes, weekend warriors, wellness seekers, and even biohackers testing out the latest diabetes technology for performance and prevention.
But here’s the question: do CGMs actually work for everyone, or only for those with a medical diagnosis?
The short answer: CGM devices are game-changing for diabetes management and prediabetes. For healthy individuals, the benefits depend on your goals, how you utilize the glucose data, and whether you have the right tools to interpret it.
This isn’t about chasing more numbers. It’s about turning real-time glucose readings into smarter decisions for food, movement, sleep, and stress.
CGMs for Non-Diabetic Users: What the Evidence Shows

Even though CGMs were designed for diabetes care, there’s a growing argument for earlier blood sugar monitoring, especially since prediabetes can linger for years undetected.1
Here’s what CGM systems can surface, even if you don’t have a diagnosis:
- Spot hidden spikes: Some “healthy people” still hit glucose levels well outside their target range after a carb-heavy meal. Standard blood glucose monitoring would miss this.
- Catch low blood sugar: Intense physical activity, certain medications, or reactive hypoglycemia can cause sudden drops in glucose levels. A real-time CGM sensor can spot lows before they become dangerous.
- Dial in nutrition: Watch how your blood glucose levels respond to specific carbohydrates, proteins, and fats, personalizing your plate beyond generic guidelines.
- Boost performance: Athletes use glucose monitoring systems to match fuel intake with energy needs and recovery windows.
- Build awareness: See how sleep quality, stress, and lifestyle changes show up in your glucose data.
Limitations and Challenges of CGM Use
That said, research on CGM use in healthy populations is still in its early stages. Most studies are small and short-term, and there’s no clear consensus yet on what an “ideal” glucose response looks like for everyone. Ultimately, CGMs can be eye-opening tools that drive positive change for some. For others, the data may feel overwhelming or not as actionable without context and guidance to pair with it.
Here are some of the most common challenges with CGM devices in folks who don’t have diabetes:2
- Cost and access: Unless you have type 1 or type 2 diabetes, insurance plans rarely cover CGM use. Out-of-pocket costs can be steep.
- Data without context: A spike isn’t “bad” unless you know what it means for glycemic control and long-term health. CGM data needs interpretation.
- Skin and tech issues: Some users get irritation or sensor failures. It’s still a medical device, not a magic patch.
- Emotional impact: Seeing every dip and climb can create food anxiety without support from a healthcare professional.
- Not always necessary: If your blood sugar levels are rock-steady and you’re symptom-free, a CGM might not add much value.
How CGMs Support Metabolic Health Beyond Diabetes
Here’s the thing: CGMs aren’t just about “diabetes management.” When you zoom out, they’re about metabolic awareness, making the invisible visible so you can see how your daily choices ripple through your blood sugar levels. Even if you’re not living with type 1 or type 2 diabetes, real-time glucose data gives you a clearer picture of what’s working (and what’s not) for your body.
Think of it as a feedback loop for your lifestyle.3
Personalized nutrition
Forget the one-size-fits-all food rules. Two people can eat the same bowl of pasta and have wildly different blood glucose responses. CGM data shows your unique glucose readings, allowing you to fine-tune portion sizes, pair carbs with protein or fiber, and identify which foods help you stay within your target range. Over time, this builds a personal nutrition playbook rooted in your biology, not generic diet trends.
Exercise feedback
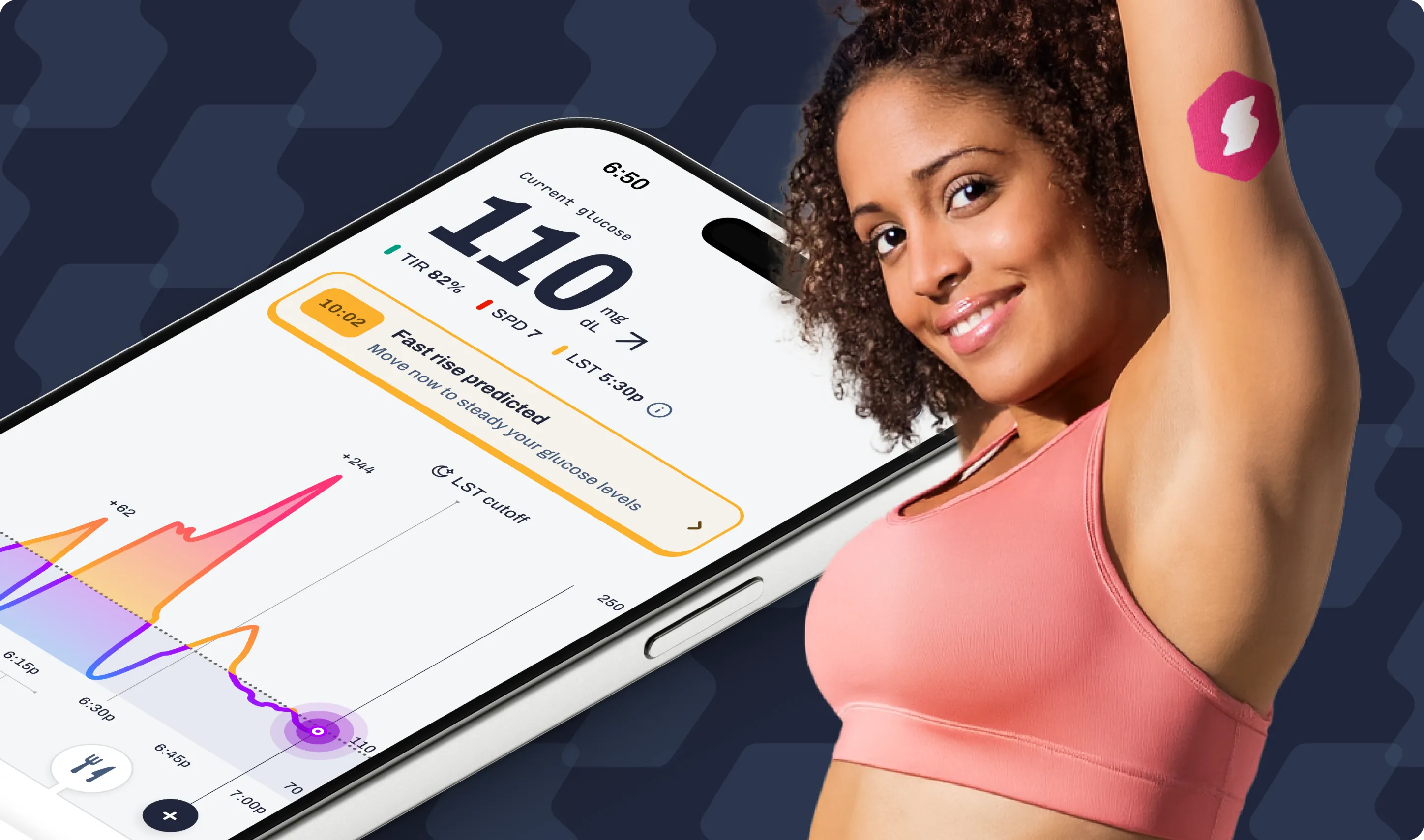
Physical activity is one of the most powerful levers for glucose control. A brisk walk after dinner can flatten a spike, while a high-intensity workout might trigger a temporary rise before recovery. With CGMs, you can see how different types of workouts (Zone 2 cardio, resistance training, or even micro-workouts) shape your glucose curve and improve your time in range.
Stress check
Cortisol is sneaky. It can drive up blood glucose levels even if you haven’t eaten. By wearing a CGM, you can literally see your “stress signature” in the data, whether that’s a work deadline spike, a sleepless night, or even emotional stress. Once you can spot the pattern, you can test interventions: breathwork, meditation, or a quick movement break.
Sleep connection
Sleep and blood sugar regulation are deeply intertwined. Poor sleep doesn’t just leave you feeling groggy; it can also lead to insulin resistance and unstable glucose levels the next day. CGMs make this visible. Compare your overnight glucose slope after a solid 8 hours versus a late-night Netflix binge, and you’ll quickly see why sleep is a metabolic superpower.
Reinforcement loop
Here’s where the magic happens. Lifestyle changes are more effective when you can see their impact in real-time. Instead of guessing whether your “healthy habit” is helping, you get proof: a flatter curve, more time in range, fewer rollercoaster spikes. That immediate feedback builds motivation, making it easier to double down on what works.
The takeaway: CGMs transform vague wellness advice into personalized metabolic feedback. They don’t just tell you what’s happening; they show you how your body reacts, moment by moment, so you can make lifestyle changes that actually last.
Future Directions and Innovations in CGM Technology
The diabetes technology space is experiencing rapid growth, led by companies such as Dexcom, Abbott (Freestyle Libre), and other FDA-cleared medical devices.
Here’s where it’s headed:
- Longer wear sensors: From 7–15 days today to months in the future.
- Smarter integrations: CGM systems syncing with wearables, fitness apps, and insulin pumps for closed-loop insulin delivery.
- AI-driven predictions: Personalized, real-time glucose forecasting based on your glucose monitoring system and lifestyle inputs.
- Over-the-counter access: FDA approval and broader availability could expand the use of CGMs beyond diabetes management into general wellness.
For those who use insulin, today’s CGMs already prevent severe low blood sugars by linking insulin pumps with CGM readings. Tomorrow’s systems? Smarter, seamless, more affordable.
Metabolic Playbook: How to Use a CGM Like a Pro
Think of a CGM as your glucose play-caller.
Here’s how to turn numbers into action:
- Pre-meal test drive: Eat a carb-heavy lunch. Watch what happens to your blood glucose levels. Adjust with more protein and fiber next time.
- Movement snacks: Walk for 10 minutes after meals to blunt spikes. CGM data will show the curve flattening.
- Sleep audit: Compare nights with 7–8 hours vs. late-night screen time. Your overnight glucose slope doesn’t lie.
- Stress intercept: Spot cortisol-driven spikes during work deadlines. Use breathwork or quick exercise as your “reset.”
- Target range focus: Don’t chase perfection. Aim for more time in range, fewer extreme highs/lows.
The Bottom Line
CGM systems are essential for people with type 1 or type 2 diabetes and are a growing tool for prediabetes management. For non-diabetic users, CGMs won’t magically deliver weight loss or perfect wellness, but they can offer valuable insight into how food, movement, and lifestyle impact blood sugar levels in real-time.
Whether you’re using a Dexcom, Abbott Freestyle Libre, or another glucose monitoring system, remember: CGMs work best when the data is paired with action.
Talk with a healthcare provider or endocrinologist before starting CGM use, especially if you take insulin or manage other conditions. With the right guidance, continuous glucose monitors can be more than just a medical device; they can serve as your daily blueprint for improved metabolic health.
Learn More With Signos’ Expert Advice
Understanding your glucose patterns is just the start; knowing what to do with that data is where real change happens. Signos combines science-backed insights with personalized guidance to help you make informed decisions about food, movement, sleep, and stress, enabling you to enhance your overall metabolic health. Learn more about glucose levels on Signos’ blog.
Topics discussed in this article:
References
1. Hegedus E, Salvy SJ, Wee CP, Naguib M, Raymond JK, Fox DS, Vidmar AP. Use of continuous glucose monitoring in obesity research: A scoping review. Obes Res Clin Pract. 2021 Sep-Oct;15(5):431-438.
2. Petrie JR, Peters AL, Bergenstal RM, Holl RW, Fleming GA, Heinemann L. Improving the clinical value and utility of CGM systems: Issues and recommendations: A joint statement of the European Association for the Study of Diabetes and the American Diabetes Association Diabetes Technology Working Group. Diabetes Care. 2017;40(12):1614-1621.
3. Ehrhardt N, Al Zaghal E. Continuous Glucose Monitoring As a Behavior Modification Tool. Clin Diabetes. 2020 Apr;38(2):126-131.



.webp)
.svg)










.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
