Key Takeaways
- Bedroom temperature affects metabolism. Sleeping in a slightly cooler room around 66°F (19 °C) can activate brown fat, improve insulin sensitivity, and support overnight glucose stability.
- Small shifts in bedroom temperature and bedding choices can meaningfully affect sleep quality, energy expenditure, and glucose levels.
- Use a continuous glucose monitor to help you personalize your ideal sleep temperature and optimize overnight glucose levels.
that {{mid-cta}}
You may not realize it, but your bedroom temperature can make or break your overnight metabolism. Sleep is a cornerstone of metabolic health, and temperature is one of its most overlooked drivers.
A cozy bed feels good, but cooler environments do more: they help stabilize glucose and improve insulin sensitivity. The ideal temperature aligns with natural circadian rhythms, supporting overnight glucose levels, fat oxidation, and deep, restorative sleep.
Finding your “sweet spot” between sleep warmth and metabolic chill can help you wake up feeling more refreshed and energized. This article will unpack how temperature influences glucose, why cooler may be better, and how Signos can help you personalize your optimal sleep environment for better overnight metabolic health benefits.
How Temperature Influences Metabolism During Sleep

Your bedroom climate doesn’t just affect comfort; it directly shapes how your body manages glucose, fat, and energy overnight.
Warmer temperatures make it harder to fall asleep and disrupt sleep quality. Shorter sleep duration, trouble falling asleep, and difficulties staying asleep make the body less responsive to insulin, increase caloric intake, and contribute to obesity, factors that worsen metabolic health and raise the risk of developing insulin resistance and type 2 diabetes.1
Cooler temperatures, on the other hand, prompt your body to generate heat, activating brown adipose tissue or brown fat. This metabolically active tissue converts calories into heat, subtly increasing energy expenditure while you sleep. Cooler sleep environments enhance brown fat activity, improve insulin sensitivity, and support glucose uptake into muscle and body fat cells, promoting overnight glucose stability and protecting you against insulin resistance.2,3,4
Some reports suggest that a chilly sleep environment can boost resting metabolic rate by 14%, raising calorie burn and substrate oxidation.4 Another study found cold exposure triggered a thermogenesis response, creating a 20% energy deficit over 24 hours, a meaningful impact on body weight loss, and metabolic health.5
Temperature also interacts with your circadian rhythm. As you fall asleep, your core temperature drops, signaling the brain for deep sleep. Skin temperature warms as core temperature cools, coinciding with melatonin release to aid sleep.4,6
Maintaining a slightly cool room supports this natural decline, helping you reach deeper sleep cycles where metabolic repair and glucose regulation occur.
Optimal Bedroom Temperature Ranges

The ideal sleep temperature isn’t one-size-fits-all. It’s a balance between comfort and metabolic benefit. While some research points to 66°F (19 °C) as optimal for activating brown fat and improving insulin sensitivity, other studies suggest a slightly broader comfort range of 68-77°F (20- 25 °C) for better sleep quality.2,7
Even small temperature shifts make a difference: For every 1°F increase in room temperature between 60 and 85°F, sleep efficiency drops by 0.06%.8 That loss in sleep quality can show up in your glucose data the next morning.7
Fine-tune your comfort at night with breathable bedding, light layers, and moisture-wicking fabrics like bamboo or linen, rather than raising the thermostat. Your body tightly regulates its temperature, keeping your skin within a specific range despite changes in external and core temperatures.9 If you tend to run cold, warm up with socks or a light blanket, but give your body time to thermoregulate as you fall into deeper sleep cycles.
The Metabolic Playbook: Strategies to Optimize Sleep Temperature

Your sleep temperature is variable. Adjusting your environment, clothing, and routine can optimize sleep temperature.
- Take a warm shower one to two hours before bed: A warm shower helps dilate blood vessels and lower core body temperature once you’re in bed, reducing the time it takes to fall asleep.10
- Adjust your bedding microclimate: Use breathable, moisture-wicking materials and layers strategically to regulate warmth as your body temperature changes overnight.9 Layer your bedding and experiment with different materials to improve your thermoregulation.
- Limit caffeine intake: Drink your last caffeinated beverage six to nine hours before bedtime to help with falling asleep. Caffeine
- Cool the air, not just your body: Ceiling or portable fans enhance airflow and help sustain a steady ambient temperature.
- Dress for thermoregulation: Lightweight, loose-fitting pajamas help maintain warmth without trapping heat. Too little clothing can leave you feeling cold, whereas too much can make you feel hot, resulting in more wakefulness and less deep and REM sleep.6
- Time your meals: Eating larger meals closer to bedtime can worsen sleep quality and contribute to circadian misalignment.11 There’s no universal rule for when to have dinner, but eating two to three hours before bed may help optimize sleep quality and circadian alignment.12
Using Signos to Track Temperature Effects on Glucose
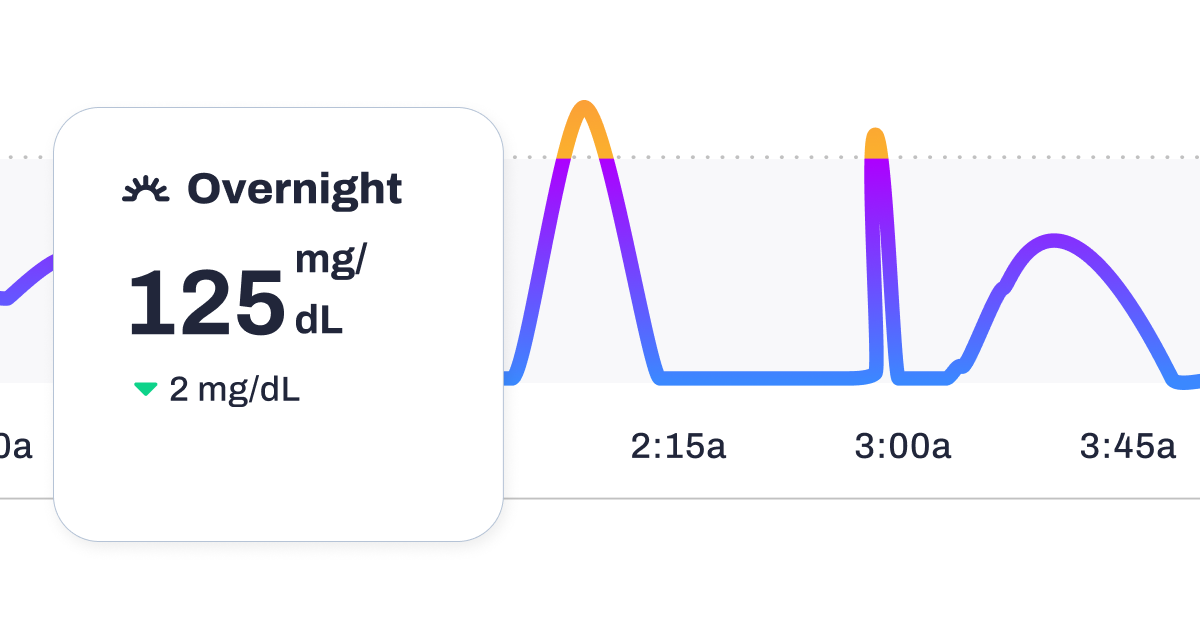
Every person’s metabolic response to temperature is unique, and Signos helps you uncover how yours shifts with environmental changes. Using continuous glucose monitoring (CGM) paired with in-app insights, you can visualize how your body reacts to hot, cold, or fluctuating temperatures.
Try these simple experiments to see how temperature affects your glucose trends:
- Cool vs. Warm Nights: Track your overnight glucose stability for a week at a slightly cooler sleep temperature (65–67°F), then compare it with a warmer week. Use your Signos CGM graph to see which environment supports more time in the purple “optimal” zone.
- Pre-Bed Chill Experiment: Try a cool shower or a few minutes of cold exposure before bed. Does your glucose stay steadier overnight?
- Workout Temperature Test: Compare a morning workout in a cool environment vs. a warm one, and review your post-workout glucose recovery curve in Signos to see how thermoregulation impacts your metabolism.
Use Signos’ in-app insights and trend analysis to identify patterns (such as reduced nighttime spikes or smoother recovery curves), and personalize your thermostat, bedding, and routine to support better metabolic balance. Over time, your data becomes your guide to optimizing both comfort and glucose stability.
The Bottom Line
A cooler bedroom can do more than make sleep comfortable; it can actively support your body’s metabolic health. For many, even small adjustments to bedroom temperature, bedding, or sleepwear can make a noticeable difference in overnight glucose stability.
With Signos, you can turn these adjustments into a personalized experiment. Combine temperature tweaks with other sleep habits, like limiting late-night carbs or experimenting with pre-bed relaxation routines, and watch how your overnight glucose curves respond. Over time, your Signos data transforms trial-and-error into actionable guidance, helping you create a sleep environment that supports both comfort and metabolic resilience.
Learn More With Signos’ Expert Advice
With Signos, you turn sleep glucose data into actionable insight unique to your body. Test small environmental tweaks and discover how your metabolism responds, creating a continuous feedback loop that guides your sleep improvement decisions. Explore the Signos blog for evidence-based guidance on glucose, energy metabolism, and sleep.
Topics discussed in this article:
References
1. https://pubmed.ncbi.nlm.nih.gov/33849816/
2. https://pubmed.ncbi.nlm.nih.gov/24954193/
3. https://pmc.ncbi.nlm.nih.gov/articles/PMC5372132/
4. https://pmc.ncbi.nlm.nih.gov/articles/PMC9273773/
5. https://academic.oup.com/jcem/article-abstract/98/7/E1218/2536785
6. https://pmc.ncbi.nlm.nih.gov/articles/PMC3427038/
7. https://pubmed.ncbi.nlm.nih.gov/37474050
8. https://academic.oup.com/sleep/article-abstract/43/Supplement_1/A464/5847198
9. https://pmc.ncbi.nlm.nih.gov/articles/PMC6491889/
10. https://pubmed.ncbi.nlm.nih.gov/32617439/




.svg)










.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
