CGMs provide reliable results in most clinical situations. The explanation, however, is not so straightforward. The reasons for this go beyond the complicated mathematics involved in comparing a new test with reference laboratory standards. The interpretation of CGM results are colored by what is measured, how often measurements are taken, when they are taken, and how the information is interpreted.
Finger prick glucometers revolutionized the management of diabetes. They allow relatively frequent measurements of blood glucose with only mild discomfort outside the confines of a doctor’s office or hospital. CGMs are another step toward empowering patients in taking a more active role in their care. By allowing patients to check their glucose status as often as they like with absolutely no pain, CGMs help individuals gain greater insight on their body’s unique responses to foods, activities, illness, and other physiological states.
Which is more accurate, a traditional glucometer or a CGM?
For starters, we have to understand that the two tests measure different things. A glucometer measures the concentration of glucose in a drop of blood by measuring the rate of a chemical reaction on a reagent strip.
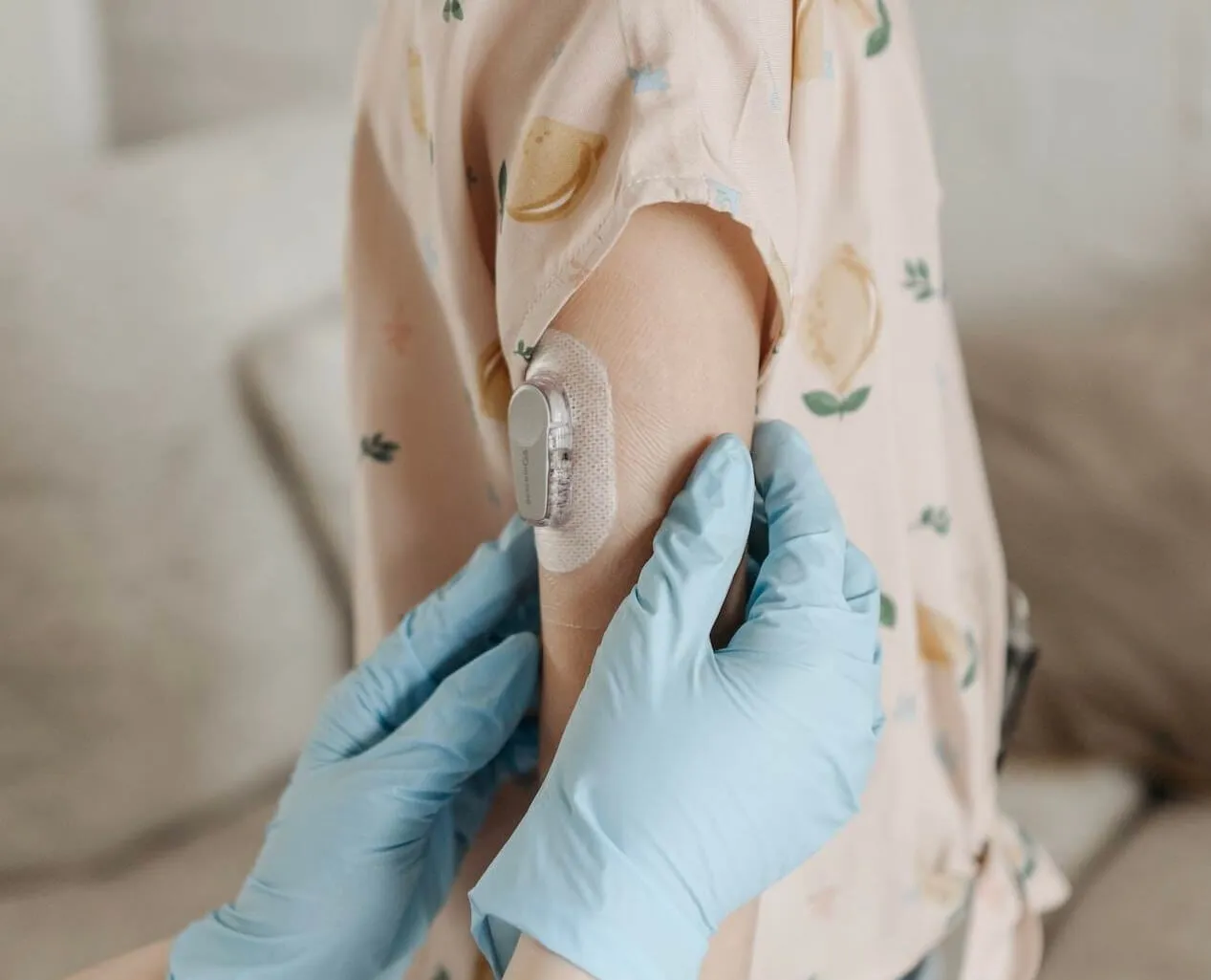
CGMs do not measure the concentration of glucose in blood. They use a tiny built-in sensor to repeatedly measure the concentration of glucose in the interstitial space – the fluid between skin cells. A reading from a CGM is actually an average of multiple samples taken.
Glucose concentrations in interstitial fluid reflect those in the blood but the two are not identical. In general, interstitial glucose lags behind blood glucose. This means that when blood sugar levels are changing rapidly (either increasing or decreasing) there will be a greater difference between results obtained from a glucometer versus those obtained from a CGM. The lag time between interstitial glucose and blood glucose levels can vary according to factors, including blood flow, but on average, the lag time is eight to ten minutes.1
Different tests; different standards. The two tests are so distinct from each other that different methods must be used to evaluate their accuracy. Finger prick glucometers are rated using International Organization for Standardization (ISO) criteria whereas CGMs are evaluated by a mathematical derivation called Mean Absolute Relative Difference (MARD). Both types of measures are compared to the gold standard benchmark: glucose concentration in a venipuncture blood sample by a credentialed reference laboratory.
Gold Standards
Tests vary in their requirement for accuracy depending on the role they play. For example, a screening test is not as reliable as a confirmatory test2. The most accurate test for a particular diagnosis is termed “the gold standard” and is typically performed by laboratories certified by organizations such as CLIA (Clinical Laboratory Improvement Amendments) or CAP (the College of American Pathologists)3. No study performed at home is considered a gold standard.
Examples of screening and confirmatory tests
Furthermore, the purpose of some tests is to help diagnose a disease, whereas other tests are used to monitor a condition we already know the patient has. Depending on the situation, clinicians will accept different levels of accuracy.
Some researchers, including Dr. Kevin Hall, have questioned the accuracy of CGM readings. To address the issue, Dr. Hall measured glucose levels in 16 hospitalized patients over a 28-day period4. The subjects were fitted with two or three CGMs produced by different manufacturers. According to the published paper’s authors, “The glucose values were significantly correlated between the CGMs (r = 0.57; P < 0.0001).” But when meals were ranked based on the glucose response measurement, there were differences between the different proprietary CGMs tested. These differences were more prominent in participants who had a higher measured body fat. And the location of the probe (abdomen versus upper arm) may have played a role in the different readings.
The researchers also noted that blood sugar levels varied when the same individual was fed the same meal one week apart. The meals were either a berry and walnut quinoa cereal or a plain bagel with cream cheese and turkey bacon. Since the glucose response to the same meal was different in subsequent weeks in the same individual, the study authors concluded that the CGMs were unreliable.
There are other possible explanations for the last observation. The same individual may experience different physiological states at different times, affecting their glucose response to a meal. Stress has been shown to affect glycemic control in patients with diabetes5. We simply don’t have good data on how exercise, sleep quality, the previous day’s meal, and stress might affect the glycemic response in patients who don’t have diabetes.
Factors That Affect Glycemic Response
Your body’s blood sugar following the ingestion of the same food can vary in different circumstances. Factors that affect glycemic response include:
- Other foods eaten. Fiber can reduce sugar absorption and blunt the glycemic response to other foods. Fat and protein slow gastric emptying and slow intestinal absorption of simple sugars.
- Cooking. Pasta prepared al dente has a lower glycemic index than overcooked spaghetti.
- Physical activity. Exercise training has been shown to reduce the insulin response to a carbohydrate meal.6
- Stress. The release of stress hormones, such as cortisol and adrenaline, alter the way your body metabolizes sugar.
Rather than discrediting CGMs, Dr. Hall’s observation seems to underline their benefits. Our physiological states are constantly changing. We cannot rely on the glycemic index listed for a particular food as a guide to blood sugar responses. Monitoring our peculiarly individual response to a meal is a much more reliable guide.
CGMs Provide Individuals With Valuable Data
.jpeg)
Biomedical research is objective and detail-oriented. Sometimes, clinicians and patients use information gleaned from rigorous studies in ways research scientists might not have expected. When this happens, the flow of information from patients to clinicians and back to clinical researchers helps guide further areas for study.
<p class="pro-tip">CGMs are so easy and painless to use, they encourage patients to take frequent readings.</p>
Many individuals will scan their CGM after trying different foods out of sheer curiosity. Sometimes, the CGM data results are eye-opening.
My wife has been using a CGM for approximately 2 years to help control her prediabetes. She has learned that eating a small portion of white rice in conjunction with a serving of vegetables has no effect on her glucose level. Tangerines and oranges barely make a dent, but a peach will cause a big spike. She was shocked to see what a huge effect eating a handful of tortilla chips can have on her.
{{mid-cta}}
A couple of days ago she called me from an airport during a stopover to tell me she bought a small bag of gummy bears as a snack. She ate a few and decided to check her CGM. The reading was 240. Gummy bears have always been one of her favorite treats. She never imagined they’d cause her sugar to spike to such a degree.
CGMs Are More Accurate Than Home Blood Glucose Monitors

CGMs are often more accurate than their predecessors. Home blood glucose monitors can be off by as much as 20%7. By obtaining samples every 10 seconds, and calculating an average of these readings every 5 minutes, in head-to-head comparisons, CGMs result in improved blood sugar control in patients with diabetes compared with the older models8.
And the future of CGMs is bright indeed. Technical improvements, the use of more sophisticated algorithms, and the incorporation of machine-learning methods will likely make CGMs increasingly versatile and reliable.
The Future of CGMs
CGMs are an established tool to help combat diabetes and improve dietary and lifestyle choices. Their use, often in conjunction with blood glucometers, provides patients with a wealth of information that helps engage them and adopt a more active role in their care. Though they do not replace the gold standard test of blood glucose measurement by venipuncture, CGMs provide reliable results in most clinical situations.
Advances in technology and developments in software design promise to make CGMs increasingly more accurate and useful in the day to day management of diabetes and other metabolic conditions.
<div class="pro-tip"><p>Read more about CGMs</p><ul><li>How CGMs Work</li><li>Scientific Evidence: CGMs for Weight Loss</li><li>Why Non-Diabetics Use CGMs</li></ul></div>
Topics discussed in this article:
References
- Cengiz, E., & Tamborlane, W. V. (2009). A tale of two compartments: interstitial versus blood glucose monitoring. Diabetes technology & therapeutics, 11 Suppl 1(Suppl 1), S11–S16. https://doi.org/10.1089/dia.2009.0002
- Maxim, L. D., Niebo, R., & Utell, M. J. (2014). Screening tests: a review with examples. Inhalation toxicology, 26(13), 811–828. https://doi.org/10.3109/08958378.2014.955932
- Heuer, C., & Stevenson, M. A. (2021). Diagnostic test validation studies when there is a perfect reference standard. Revue scientifique et technique (International Office of Epizootics), 40(1), 261–270. https://doi.org/10.20506/rst.40.1.3223
- Howard, R., Guo, J., & Hall, K. D. (2020). Imprecision nutrition? Different simultaneous continuous glucose monitors provide discordant meal rankings for incremental postprandial glucose in subjects without diabetes. The American Journal of Clinical Nutrition, 112(4), 1114–1119. https://doi.org/10.1093/ajcn/nqaa198
- Lloyd, C. E., Dyer, P. H., Lancashire, R. J., Harris, T., Daniels, J. E., & Barnett, A. H. (1999). Association between stress and glycemic control in adults with type 1 (insulin-dependent) diabetes. Diabetes care, 22(8), 1278–1283. https://doi.org/10.2337/diacare.22.8.1278
- Lambert, C. P. (2018). Exercise training alters the glycemic response to carbohydrate and is an important consideration when evaluating dietary carbohydrate intake. Journal of the International Society of Sports Nutrition, 15(1). https://doi.org/10.1186/s12970-018-0259-2
- Ekhlaspour, L., Mondesir, D., Lautsch, N., Balliro, C., Hillard, M., Magyar, K., Radocchia, L. G., Esmaeili, A., Sinha, M., & Russell, S. J. (2016). Comparative Accuracy of 17 Point-of-Care Glucose Meters. Journal of Diabetes Science and Technology, 11(3), 558–566. https://doi.org/10.1177/1932296816672237
- Janapala, R. N., Jayaraj, J. S., Fathima, N., Kashif, T., Usman, N., Dasari, A., Jahan, N., & Sachmechi, I. (2019). Continuous Glucose Monitoring Versus Self-Monitoring of Blood Glucose in Type 2 Diabetes Mellitus: A Systematic Review with Meta-analysis. Cureus. https://doi.org/10.7759/cureus.5634




.svg)









.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
