Key Takeaways
- Glucose variability, not just high glucose, is a key driver of energy crashes and fatigue.
- Fall’s shorter days and heavier meals make glucose control harder to manage.
- Stable meals, movement, and sleep routines are the best ways to sustain energy.
{{mid-cta}}
Feeling sluggish this time of year is common. Work and social calendars ramp up in the fall, and most people already start mentally prepping for the holidays. On top of this, it gets darker earlier, which naturally impacts your circadian rhythm, causing you to feel more tired compared to the long sunny days of summer.
While the decreased daylight and busier schedules may play a role in feeling fatigued, there is a less obvious factor that may be quietly draining your energy: glucose variability and blood glucose fluctuations. Unlike fasting glucose or HbA1C, which capture averages of blood glucose levels, glycemic variability reflects how much your glucose oscillates throughout the day, a key predictor of fatigue and long-term metabolic health.
Research shows that frequent highs (episodes of hyperglycemia) and lows (hypoglycemia) in blood sugar, even in people without type 2 diabetes mellitus, can increase oxidative stress, damage mitochondria, and impair energy metabolism.1,2
In other words, your glucose excursions and glycemic excursions might be the reason you’re feeling sluggish, foggy, and reaching for extra coffee this season.
What Is Glucose Variability?
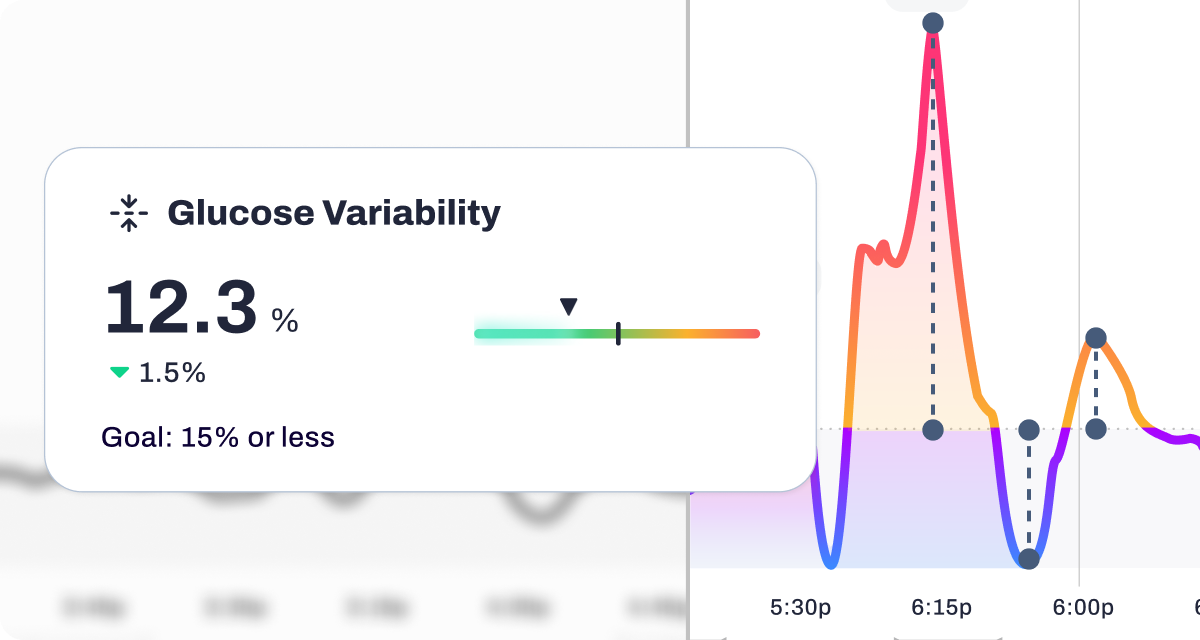
Glucose variability (GV) refers to the degree of fluctuation in blood glucose levels over time. GV is often measured using the mean amplitude of glycemic excursions (MAGE), standard deviation, or coefficient of variation from continuous glucose monitoring (CGM) data.3
While a stable HbA1C might look reassuring, it represents your mean glucose or average glucose, and doesn’t show short-term postprandial spikes or nadirs. Two people can share the same average but have vastly different outcomes depending on their glycemic variation and time in range.
Studies indicate that greater glycaemic variability, not just elevated glucose averages, is linked to an increased risk of endothelial dysfunction, macrovascular complications, and cardiovascular disease.4,5
Simply put, it’s not just high vs. low blood glucose, but how fast it swings that matters in diabetes management and overall healthcare.
How Blood Sugar Swings Drain Energy

When postprandial glucose spikes rapidly after a meal, insulin levels rise to bring it down. The sharp drop that follows (sometimes dipping into low blood glucose) creates fatigue, irritability, and brain fog.
This pattern of short-term GV has been shown in PubMed-indexed studies to elevate oxidative stress and inflammation within mitochondria.6 Mitochondria depend on stable glycemia for consistent energy production.
Over time, these glucose fluctuations contribute to insulin resistance, chronic hyperglycemia, and an increased risk of both microvascular complications (such as nephropathy and diabetic retinopathy) and macrovascular complications.
The Seasonal Angle: Why GV Matters More in Fall
Fall introduces a perfect storm for unhealthy glucose profiles and glycemic excursions. Shorter days reduce sunlight exposure, which can impair insulin sensitivity and alter appetite-regulating hormones.7
At the same time, carb-heavy comfort foods and lower activity can trigger high GV and reduced time in range, especially in type 2 diabetic patients or those with prediabetes.
Even nondiabetic individuals experience glycemic variability and fatigue during this time of year, making continuous glucose monitoring data particularly useful for identifying risk factors in real-time.
Signs Glucose Variability May Be Driving Your Fatigue
-min.png)
Most people blame lack of sleep when they experience daytime fatigue, but if you notice any of these patterns, high GV or unstable glucose control may be the cause.
- Afternoon energy crashes, even after a full night’s rest
- Brain fog or difficulty concentrating during the day
- Energy drops one to two hours after eating
- Caffeine dependence or intense sugar cravings
Tracking these signs alongside CGM data or self-monitored blood glucose (SMBG) readings can help identify patterns and guide clinical practice.
The Metabolic Playbook: Stabilizing Energy This Fall

Fortunately, minimizing glucose variability doesn’t require extreme diets or big measures. The small, consistent habits below can help maintain energy throughout the day:
- Balance every meal with protein, fiber, and fat. These slow the absorption of carbohydrates and prevent sharp spikes.
- Opt for low-glycemic carbs such as lentils, quinoa, or sweet potatoes over refined grains.
- Move after meals. Even as little as a 10-minute “movement snack” can lower post-meal glucose jumps.
- Prioritize consistent sleep. Stable circadian rhythms improve insulin sensitivity and hormone balance.
- Manage stress. Elevations in the stress hormone cortisol can trigger both insulin resistance and cravings.
- Hydrate consistently. Dehydration can concentrate blood glucose and intensify fatigue.
Using Signos to Track and Improve Energy Stability

Signos combines real-time continuous glucose monitoring with personalized insights to help you understand your glucose profiles and glycemic control.
These data-driven insights empower better diabetes management and support both endocrine and metabolic health. Below are some of the benefits of using the Signos AI-powered app:
- Monitor Daily Spikes: See how meals and activity influence your glucose values in real time.
- Time-in-Range Metrics: Identify when your glucose remains stable and when it fluctuates.
- Personalized Insights: Receive recommendations for meal timing and food composition.
- Context Logging: Note energy levels, stress, and sleep to spot correlations in glucose patterns.
By pairing your metabolic data with daily behaviors, you can finally pinpoint what’s driving your fall fatigue and fix it at the source.
The Bottom Line
Fall fatigue isn’t just in your head. While various factors contribute, unexplained tiredness often stems from glycemic variability, a pattern linked to oxidative stress, autonomic neuropathy, and cardiovascular risk.
By understanding your CGM data, glucose values, and time in range, you can improve glycemic control and reduce the risk of hypoglycemia.
With Signos, real-time CGM insights transform vague fatigue into actionable data for better long-term outcomes.
Learn More With Signos’ Expert Advice
Signos combines cutting-edge research with the proven benefits of continuous glucose monitoring data to help you achieve your health goals. Check out more articles on the Signos blog.
Topics discussed in this article:
References
- Saisho Y. Glycemic variability and oxidative stress: a link between diabetes and cardiovascular disease?. Int J Mol Sci. 2014;15(10):18381-18406. Published 2014 Oct 13. doi:10.3390/ijms151018381
- Ceriello A, et al. Oscillating Glucose Is More Deleterious than Sustained High Glucose: Effects on Endothelial Function. Diabetes. 2008;57(5):1349-1358.
- Lazar S, Ionita I, Reurean-Pintilei D, Timar B. How to Measure Glycemic Variability? A Literature Review. Medicina (Kaunas). 2023;60(1):61. Published 2023 Dec 28. doi:10.3390/medicina60010061
- Zhou Z, Sun B, Huang S, Zhu C, Bian M. Glycemic variability: adverse clinical outcomes and how to improve it?. Cardiovasc Diabetol. 2020;19(1):102. Published 2020 Jul 4. doi:10.1186/s12933-020-01085-6
- Monnier L, Mas E, Ginet C, et al. Activation of Oxidative Stress by Acute Glucose Fluctuations Compared With Sustained Chronic Hyperglycemia in Patients With Type 2 Diabetes. JAMA. 2006;295(14):1681–1687. doi:10.1001/jama.295.14.1681
- Zhang Z, Huang Q, Zhao D, Lian F, Li X, Qi W. The impact of oxidative stress-induced mitochondrial dysfunction on diabetic microvascular complications. Front Endocrinol (Lausanne). 2023;14:1112363. Published 2023 Feb 7. doi:10.3389/fendo.2023.1112363
- Mina Bahrami, Makan Cheraghpour, Sima Jafarirad, Pejman Alavinejad, Bahman Cheraghian; The role of melatonin supplement in metabolic syndrome: A randomized double blind clinical trial. Nutrition & Food Science 3 September 2019; 49 (5): 965–977. https://doi.org/10.1108/NFS-01-2019-001




.svg)










.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
