Key Takeaways
- GLP-1 side effects can be intense, which is why microdosing GLP-1 medications has become more common.
- Long-term research is limited, though there are potential benefits and risks associated with low-dose GLP-1.
- Lifestyle factors can support metabolic health, either in addition to or instead of GLP-1s.
that {{mid-cta}}
Microdosing GLP-1 medications has become a popular trend. Borrowed from the world of psychedelics, microdosing now refers to taking smaller-than-standard doses of GLP-1s in an attempt to reduce side effects and medication costs. But is this clever biohacking or risky guesswork?
This guide explains what microdosing GLP-1s means, potential benefits and risks, and how tools like Signos can help you safely monitor and optimize your metabolic health while using these medications.
What Does Microdosing GLP-1 Mean?

Microdosing involves taking a smaller dose of a GLP-1 drug, such as semaglutide (Wegovy, Ozempic, Rybelsus) or tirzepatide (Mounjaro, Zepbound).
Why people try it:
- Reduce gastrointestinal side effects like nausea or vomiting
- Make dose adjustments easier when switching medications1
- Stretch prescription supply or reduce cost
Because microdosing is considered an off-label use, it’s important to understand both the potential benefits and the unknowns.
How GLP-1 Medications Work

GLP-1 (glucagon-like peptide-1) is a hormone naturally produced in your gut that can promote feelings of fullness, slows digestion, and help release insulin. These effects are why GLP-1 agonist medications have seen increased popularity, particularly in the weight-loss industry. Originally, GLP-1 medications were intended to treat people living with type 2 diabetes.2 FDA-approved dosing protocols exist to maximize safety and effectiveness:
- Subcutaneous semaglutide (Wegovy/Ozempic): Start at 0.25 mg weekly for 4 weeks, increase gradually to a maximum of 2 mg.
- Oral semaglutide (Rybelsus): Start at 3 mg daily for 30 days, increase to 7 mg, then up to 14 mg max.3
- Tirzepatide (Mounjaro/Zepbound): Start at 2.5 mg weekly, increase every 4 weeks to a maximum of 15 mg.4
Potential Benefits of Microdosing

While research on microdosing GLP-1 is limited, some potential advantages include:
- Reduced GI side effects such as nausea
- Easier adaptation to the medication, promoting longer-term adherence
- Financial savings from a slower prescription ramp-up
- Milder appetite suppression without the full-dose side effects1
Risks and Unknowns of Microdosing
Because microdosing is not yet studied extensively:
- Long-term effects on weight, metabolism, and appetite are unclear
- Lack of standardized protocols means outcomes can vary widely
- Improper dosing could lead to weight plateaus or regain
It’s crucial that patients considering microdosing do so under medical supervision. Without official standards in place, clinics can choose to practice microdosing differently. In addition, both patients and healthcare providers need to be educated on how to do it correctly to ensure the patient’s safety.1
Complementary Strategies for Metabolic Health

Even with a GLP-1, lifestyle habits remain foundational to lasting results. Medications can support weight loss and appetite regulation, but daily choices still shape long-term metabolic health. Signos makes it easy to test how these habits (and your GLP-1 dose) work together in real time.
Nutrition
Balanced meals with protein, carbs, and non-starchy vegetables help manage post-meal glucose spikes. Diets like the Mediterranean Diet can support overall metabolic health.5
Try this with Signos:
- Meal Sequencing Experiment: Eat the same meal twice: once with carbs first, once ending with protein and vegetables. Compare glucose curves to see how food order affects your response while on your GLP-1.
- Dose Day vs. Non-Dose Day: Log your meals on a GLP-1 injection day and a non-injection day. Look for changes in glucose stability or meal timing driven by differences in appetite.
- Fiber Focus: Add a high-fiber side (like lentils or broccoli) to a typical meal and watch how it impacts your post-meal glucose rise.
Exercise
Cardio lowers glucose levels in the moment, while strength training builds muscle that improves how your body stores and uses glucose long-term.
Try this with Signos:
- Pre- vs. Post-Meal Movement: Compare your glucose after a 10-minute walk before eating versus after eating. See which flattens your curve more effectively while on your GLP-1.
- Strength Training Days: Track how glucose patterns differ on strength-training days versus rest days to understand how muscle activity affects your glucose control.
Sleep
Getting 6–8 hours of quality sleep each night supports metabolic function. Studies show that sleeping less than 6 hours or more than 8 hours is linked with an increased risk of metabolic syndrome.6
Try this with Signos:
- Sleep Quality Test: Compare overnight glucose trends between nights of good sleep and poor sleep. Look for stability in your overnight glucose plateau (usually shown as a smooth purple line in Signos).
- Bedtime Routine Experiment: Adjust your evening habits (like reducing screen time or eating earlier) and watch how it affects your overnight glucose and morning fasting levels.
How Signos Helps You Decide and Adapt
When you combine GLP-1 therapy with these lifestyle experiments, you start to see how daily habits amplify (or sometimes counteract) your medication’s effects. Signos helps you capture that full picture, translating moment-to-moment glucose patterns into actionable insight.
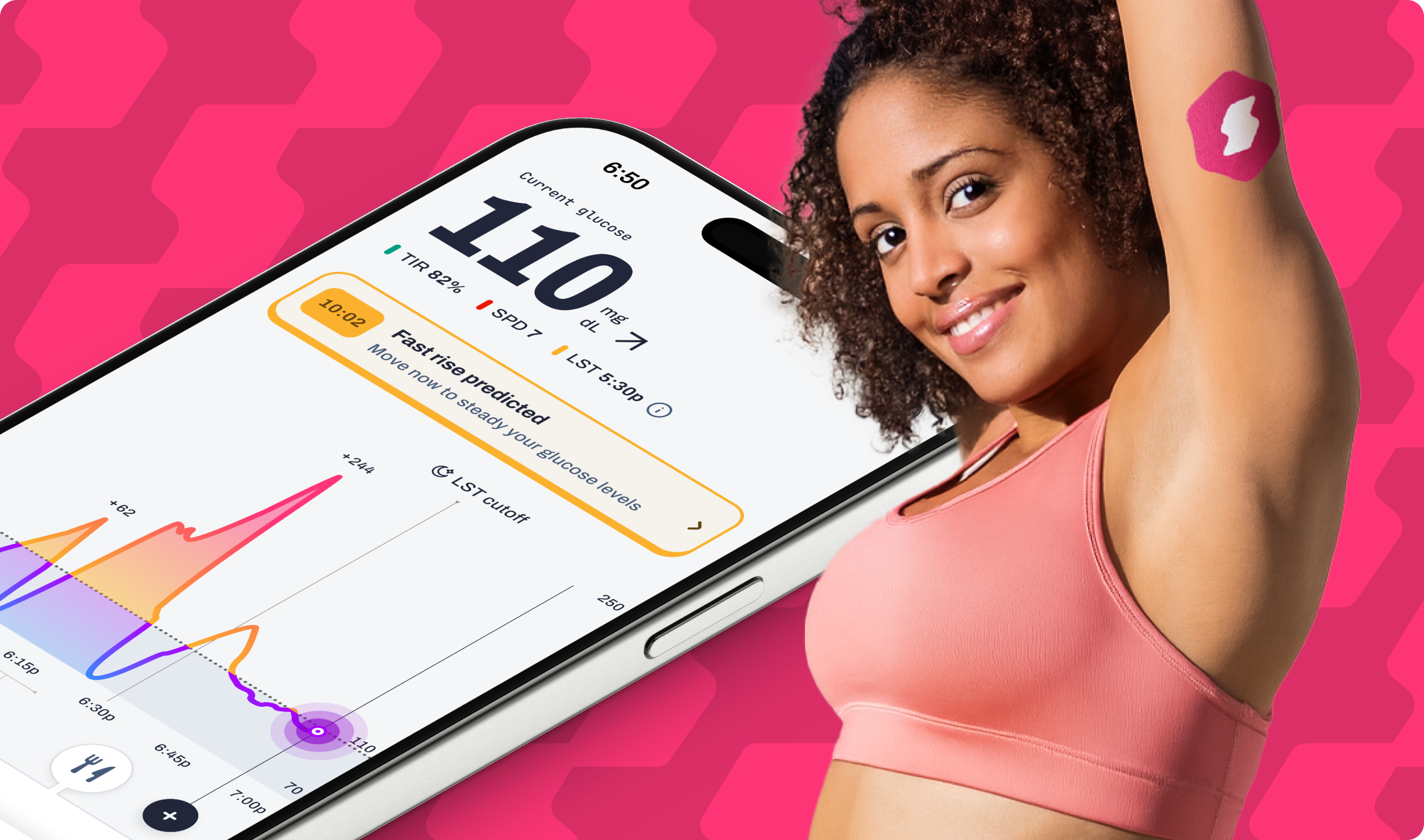
Continuous glucose monitoring (CGM) with Signos is a game-changer for anyone on a GLP-1, whether you’re starting, adjusting doses, or exploring microdosing:
- Track your body’s response to each dose: See how a lower dose or higher doses affect glucose stability, appetite, and energy in real time.
- Optimize habits alongside medication: Use your data to identify which foods, workouts, and sleep patterns support steadier glucose and stronger results.
- Support safe, data-driven adjustments: Share your Signos insights with your provider to help fine-tune your dose and manage potential side effects.
Over time, this combination of CGM data and behavioral feedback helps you move beyond medication dependence toward metabolic awareness and long-term health.
The Bottom Line
Microdosing GLP-1 may reduce side effects or stretch prescriptions, but it’s not yet an evidence-based shortcut. The safest, most effective approach combines medication with real-time metabolic tracking and healthy lifestyle habits.
Signos helps you understand your body’s response to GLP-1 doses, optimize your metabolic health, and build long-term habits that go beyond medication.
Learn More With Signos’ Expert Advice
Signos combines glucose monitoring with support from registered dietitians to help you improve your metabolic health. To learn more about how glucose impacts health, visit the Signos blog.
Topics discussed in this article:
References
- Komé, A. M., Chandran, M. M., Tungate Lopez, S. S., Buse, J. B., & Klein, K. R. (2025, February 20). One size does not fit all: Understanding microdosing semaglutide for diabetes in multidose pens. Diabetes Care, 48(3), e25–e27. doi:https://doi.org/10.2337/dc24-2575
- Hammad, B. F., Zafar, N., Ullah, M., Faisal, S. J., Iftikhar, F., Waheed, H., Mufazzar, M. W., Ahmed, K., Ashraf, F., Zahid, K., Akhtar, M., & Elijack, M. M. F. (2025, July 9). Exploring the multifaceted roles of GLP-1 receptor agonists; a comprehensive review. Front. Clin. Diabetes Healthc, 6. doi:https://doi.org/10.3389/fcdhc.2025.1590530
- Kommu S, Whitfield P. Semaglutide. [Updated 2024 Feb 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK603723/
- Farzam K, Patel P. Tirzepatide. [Updated 2024 Feb 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK585056/
- Papadaki, A., Nolen-Doerr, E., & Mantzoros, C. S. (2020). The effect of the Mediterranean Diet on metabolic health: A systematic review and meta-analysis of controlled trials in adults. Nutrients, 12(11), 3342. doi:https://doi.org/10.3390/nu12113342
- Che, T., Yan, C., Tian, D., Zhang, X., Liu, X., & Wu, Z. (2021). The association between sleep and metabolic syndrome: A systematic review and meta-analysis. Frontiers in endocrinology, 12, 773646. doi:https://doi.org/10.3389/fendo.2021.773646




.svg)










.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
