Key Takeaways
- Insulin resistance often develops silently for over a decade before presenting as prediabetes or type 2 diabetes.
- Subtle shifts, such as fatigue, energy crashes, mood swings, cravings, and abdominal weight gain, can serve as early warning signals and help spur lifestyle changes to reverse insulin resistance.
- Tracking glucose patterns with a CGM enables you to detect metabolic changes, identify problematic behaviors, and make actionable adjustments to protect your long-term metabolic health.
that {{mid-cta}}
People often expect to see or feel obvious signs of insulin resistance, but in reality, the condition typically develops silently over the years.
However, the body does provide early, non-obvious signs. Learning to recognize those subtle shifts can help you take action before blood sugar levels rise and insulin resistance develops.
In this article, you will discover the hidden signs of insulin resistance and how tracking with Signos to monitor glucose patterns can help catch it early and optimize long-term metabolic health.
What Is Insulin Resistance?

Insulin resistance occurs when the body doesn’t respond to insulin like it should. When functioning properly, insulin is a hormone produced by the pancreas that helps the body use energy properly.1
After you eat or drink foods containing carbohydrates, the digestive system breaks them down into glucose (sugar), which is then released into the bloodstream. Insulin is released from the pancreas in response to increased blood sugar levels.2
Insulin enables cells to take up glucose from the blood, lowering blood glucose levels as the glucose is used for energy. Blood sugar levels change throughout the day in response to activities like eating and physical activity.2
When your blood sugar levels stay consistently elevated, it indicates that something in the process is malfunctioning, whether due to biological factors, diet, or a lack of physical activity. If blood glucose continues to rise, it can lead to prediabetes or type 2 diabetes. Your blood sugar level reflects how effectively your body converts food into energy.1
About 87 million American adults are living with prediabetes or type 2 diabetes and don’t know it; that's about one in four U.S. adults. Prediabetes increased the risk of developing type 2 diabetes, metabolic syndrome, heart disease, and stroke. Without lifestyle changes, more than 70% of people with prediabetes will progress to type 2 diabetes.3
Certain risk factors are associated with insulin resistance (and prediabetes), including:
- Excess weight or a larger waist size
- Being 35 years or older
- Family history of diabetes
- Being African American, American Indian, Asian American, Hispanic, Latino, or Pacific Islander
- Physical inactivity (sedentary lifestyle)
- Smoking or being exposed to secondhand smoke
- History of gestational diabetes, or giving birth to a baby weighing 9 pounds or more
- Having other conditions like PCOS, Cushing’s syndrome, acromegaly, sleep apnea, or a viral disease like COVID-19
- Taking certain medications over time (glucocorticoids, antipsychotics, and HIV medications)4
While you can’t change some of these risk factors, you can make lifestyle changes, such as improving your diet and sleep, managing stress, and increasing physical activity, to reduce many of them and help prevent the metabolic complications of insulin resistance. Keep in mind that most causes of insulin resistance are from external factors that you can modify and control.4
Beyond Blood Sugar: Subtle Signs Your Body Is Becoming Insulin Resistant

In addition to risk factors for developing insulin resistance, look out for subtle signs that your body is not handling energy optimally and is becoming insulin resistant.
- Fatigue and Energy Crashes: These symptoms can be caused by progressive insulin resistance. When you provide your body with too much fuel (food), the muscles, liver, and fat tissue become less responsive to insulin, which causes the fuel (glucose) to remain in the bloodstream instead of being transferred to the cells that need energy to function optimally.4 Energy crashes can occur when you consume an abundance of simple carbohydrates, which lead to insulin and glucose spikes, followed by subsequent crashes, as they don’t provide sustained energy.1
- Stubborn Weight Gain: Research shows that abdominal weight gain (or visceral fat), along with fat storage in the liver and muscles, leads to insulin resistance and type 2 diabetes through inflammation and disrupted insulin signaling. Weight gain distributed evenly throughout the whole body is less risky than abdominal fat, which can interact with your organs.5
- Skin Changes: Pay attention to dark patches (acanthosis nigricans) and skin tags. Acanthosis nigricans is a velvety darkening of the skin, usually in skin folds (the back of the neck, armpits, or groin), caused by increased insulin levels that activate skin cells to multiply rapidly. Skin tags can also occur.6
- Cravings and Hunger Swings: Research suggests that insulin resistance also affects the brain, making it harder to resist cravings compared to individuals without insulin resistance.7
- Brain Fog and Mood Swings: The brain prefers glucose as its primary energy source, so fluctuations in blood sugar can impact mood, focus, and cognitive performance. Low blood sugar levels or blood sugar swings can cause irritability, poor mood, and trouble concentrating.8 Studies using continuous glucose monitoring in women with type 2 diabetes show that big swings in glucose are associated with lower quality of life and negative moods.9
- Poor Sleep or Night Sweats: Even a single night of partial sleep deprivation increases insulin resistance; continued poor sleep (including night sweats) could further worsen the effect. Short sleep duration is associated with a higher risk of obesity and type 2 diabetes.11
Why These Symptoms Matter: The Hidden Metabolic Story

If you notice symptoms like fatigue, energy crashes, and skin changes, think of them as your body's early “check engine lights” indicating that your metabolic health needs attention.
Catching these signals early gives you the chance to prevent insulin resistance from getting worse and affecting other systems in your body. Insulin resistance typically develops 10 to 15 years before the onset of type 2 diabetes.4
Insulin resistance doesn’t act alone; it’s part of a complex web of interactions. Inflammation, stress hormones such as cortisol, and other hormonal imbalances can all contribute to insulin resistance, exacerbating each problem over time.4
Chronic stress (often marked by elevated cortisol) and inflammation can make your body less sensitive to insulin.11
Women with PCOS have a significantly increased risk of insulin resistance, abnormal lipid levels, type 2 diabetes, heart disease, and altered glucose metabolism. The hormonal changes during perimenopause can also predispose women to insulin resistance, leading to metabolic changes.12
Factors outside your control can impact your metabolic health, but paying attention to warning signs and making lifestyle adjustments can help you achieve optimal insulin function and overall well-being.
How to Detect and Track Insulin Resistance Early

Insulin resistance is commonly diagnosed with key lab markers, including:12
- Fasting insulin level (usually fasting for 8 to 12 hours, a high level may indicate insulin resistance)
- HOMA-IR is a calculation of fasting glucose and fasting insulin to estimate insulin resistance
- A1C is a measure of average blood sugar over the past 2 to 3 months. If elevated, it can indicate prediabetes and type 2 diabetes, which often develop after insulin resistance.
- High glucose variability contributes to the development of insulin resistance.13
For even earlier detection, CGM data can help provide further insight into your glucose variability and glucose responses to food, drinks, physical activity (or lack thereof), stress, and sleep patterns.
It can detect patterns that precede elevated lab markers, helping you to strengthen your lifestyle habits and prevent further metabolic issues and stress, such as insulin resistance. Catching behaviors early gives you the chance to adjust them before they become hard-to-break habits.
How Signos Helps You Catch the Early Signals
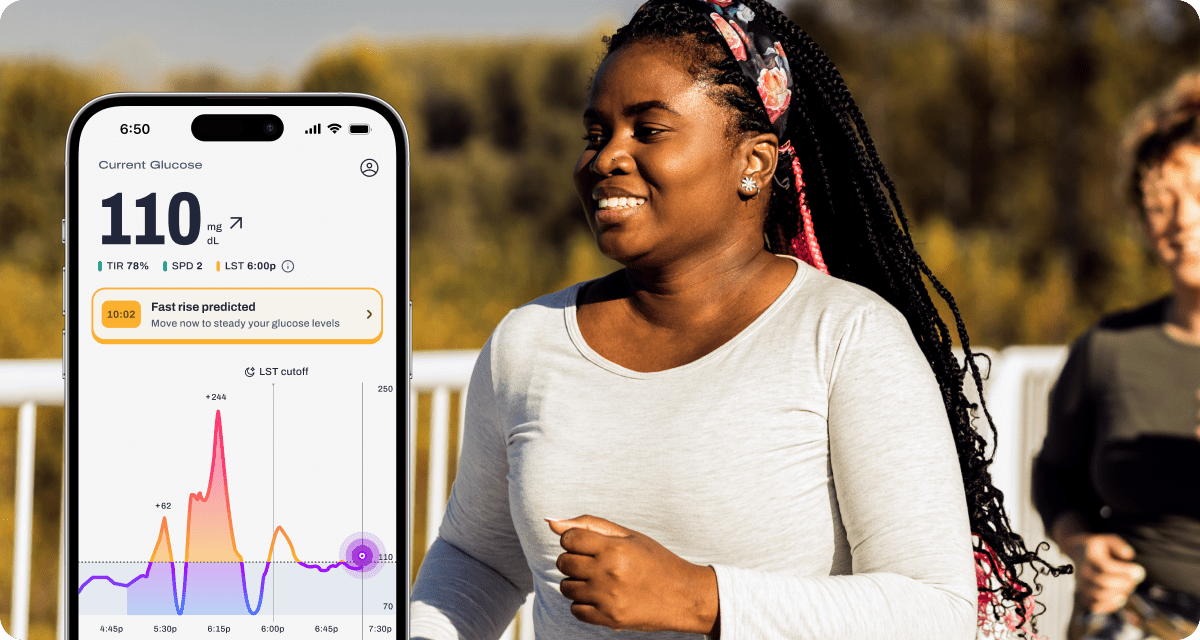
Insulin resistance rarely shows up overnight; your glucose patterns reveal it long before lab work does. Signos makes those early shifts visible by turning a continuous glucose monitor (CGM) into a daily feedback loop that helps you understand what’s driving instability and what brings you back into balance.
Signos CGM Features & How They Support Early Detection
- Real-time glucose tracking to reveal subtle instability. Signos shows your glucose line minute-to-minute, making it easy to spot early signs like elevated fasting levels, frequent mini-spikes from snacking, or slow returns to baseline after meals: all common markers of reduced insulin sensitivity.
- Pattern recognition across meals, movement, stress, and sleep. Because the Signos app layers your glucose data with lifestyle inputs, you can quickly see which habits are helping or hindering your metabolic response.
- Intelligent nudges that guide corrective action in the moment. Signos offers personalized prompts to help stabilize glucose before the spike escalates, such as a movement suggestion after a higher-impact meal or a reminder to pair carbs with protein or fiber next time. These micro-adjustments build the habits that support insulin sensitivity over time.
Experiments You Can Try in the Signos App
These experiments help reveal early signs of insulin resistance while showing you what improves your response:
- Carb-Pairing Experiment: Eat a high-carb meal alone, then repeat it paired with protein or fiber. Compare the spike size and recovery time in the app.
- Sleep-Impact Check: Log a night of shorter or disrupted sleep, then notice if next-day meals produce bigger or longer spikes. This highlights how sleep quality affects insulin sensitivity.
- Stress-vs-Stability Experiment: Tag a stressful event in the app and monitor whether your glucose drifts upward afterward. Try a 10-minute walk or breathing exercise and watch how quickly you return to baseline.
- Movement Timing Test: Eat a typical meal twice: once without movement, once followed by a brief post-meal walk. Track how your glucose curve shifts and whether recovery speeds up.
- Late-Night Eating Experiment: Compare your response to the same meal eaten earlier vs. later in the evening. A sharper or longer spike at night is a classic early indicator of insulin resistance.
A CGM isn’t just a glucose-tracking device; it’s an early-detection system. Paired with Signos’ insights and experiments, you can spot drifting insulin sensitivity long before it becomes a problem and take action with confidence.
The Bottom Line
Insulin resistance usually develops gradually, but early signs, such as fatigue, cravings, stubborn belly fat, and energy crashes, can signal that something may be amiss.
Tracking your body’s glucose response with tools like Signos helps you catch these patterns early, giving you the chance to adjust meals, activity, and lifestyle before habits become hard to break. By paying attention to these warning signals, you can protect your metabolic health and reclaim energy, clarity, and balance.
Learn More With Signos’ Expert Advice
The Signos app helps you monitor your personalized metabolic insights, enabling you to make adjustments and catch the earliest warning signals, and helps you improve your overall health. Learn more about glucose levels and tracking on the Signos blog, written by health and nutrition experts.
Topics discussed in this article:
References
- https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance
- https://www.hsph.harvard.edu/nutritionsource/carbohydrates/carbohydrates-and-blood-sugar/
- https://www.cdc.gov/diabetes/prevention-type-2/prediabetes-prevent-type-2.html?CDC_AAref_Val=https://www.cdc.gov/diabetes/basics/prediabetes.html
- https://www.ncbi.nlm.nih.gov/books/NBK507839/
- https://pubmed.ncbi.nlm.nih.gov/22327367/
- https://www.ncbi.nlm.nih.gov/books/NBK431057/
- https://pubmed.ncbi.nlm.nih.gov/25795413/
- https://pubmed.ncbi.nlm.nih.gov/12034132/
- https://pubmed.ncbi.nlm.nih.gov/22324383/
- https://pubmed.ncbi.nlm.nih.gov/16227462/
- https://pubmed.ncbi.nlm.nih.gov/35368460/
- https://pubmed.ncbi.nlm.nih.gov/24092831/
- https://pubmed.ncbi.nlm.nih.gov/31707004/




.svg)










.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
.svg)
